
In-network providers can utilize NaviNet®  to check eligibility and benefits for Highmark Blue Cross Blue Shield of Western New York members. The following message or similar may appear when you view a member’s benefits within NaviNet or HEALTHeNET indicating that authorizations are required for every outpatient/inpatient service (screenshot below).
to check eligibility and benefits for Highmark Blue Cross Blue Shield of Western New York members. The following message or similar may appear when you view a member’s benefits within NaviNet or HEALTHeNET indicating that authorizations are required for every outpatient/inpatient service (screenshot below).
However, prior authorizations are not required for every service, procedure and/or durable medical equipment, prosthetics, orthotics and supplies (DMPOS). Please check the “Prior Authorization Code Lists” to ensure an authorization is needed prior to performing the procedure or service.*
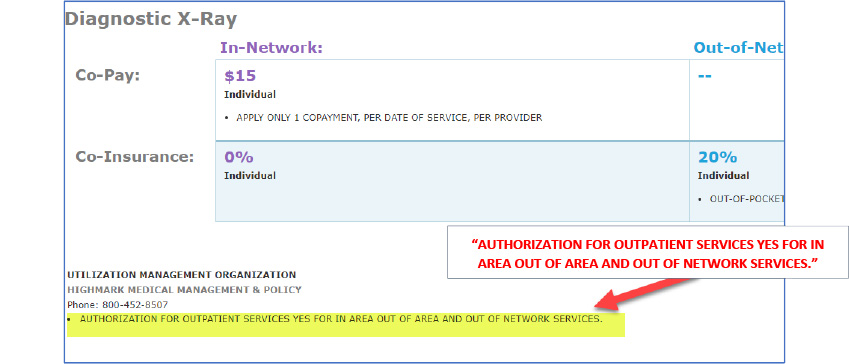
*NOTE: Authorization requirements can vary by member contract (some groups do not require every authorization on this list). You may check a member's specific authorization requirements by calling the precertification number on the back of their card.